The Centers for Medicare and Medicaid Services (CMS) asserts it has the right to deny paying for a treatment if a settlement recipient still has funds in a Medicare Set Aside (MSA) or has not properly reported their full exhaustion of those funds. Some attorneys, adjusters and injured parties have questioned over the years - is Medicare really denying bills? The truth is that Medicare is issuing denials.
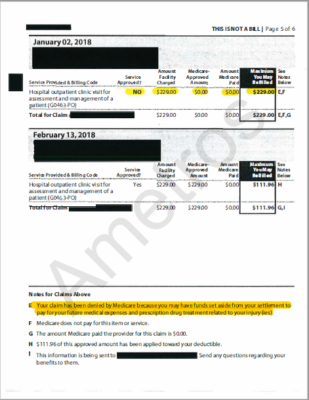
Below is an image of a true denial letter from CMS. The following document is a Medicare Summary Notice sent to a Medicare beneficiary. On page 2, you can see that a service was not approved, and looking at footnote E, CMS explains:
“Your claim has been denied by Medicare because you may have funds set aside from your settlement to pay for your future medical expenses and prescription drug treatment related to your injury(ies).”
In this instance, a man settled his case in 2014, without a professional administrator. Unfortunately, he did not spend his MSA funds in accordance with CMS guidelines. He was receiving denial letters from Medicare, and they were not paying for treatment, so he reached out to us asking for help.
This document shows that CMS is becoming savvier and denying treatments that should be paid for with settlement funds. Injured parties that do not expend their settlement funds appropriately are at risk of jeopardizing their future Medicare benefits.
Do you have questions about Medicare compliance? Reach out to us!