Get in Touch with Ametros
Your Settlement Experts
At Ametros, we make it easy for you to get the support you need. Whether you need assistance managing a medical fund, have questions about a settlement, or are looking for expert support for your clients, our team is ready to help. Fill out the form below, call us, or email us, we're here to help you every step of the way.
Contact Us
Your Local Ametros Representative
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- DC
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming
What Our Members & Partners Are Saying

I now have a life because of Ametros, and I can't thank them enough.
CareGuard Member
Watch the video!

Everyone is so caring when speaking with me that I wish all companies ran like CareGuard. Exceptional service and staff. I rate you guys at a 10. Thanks for caring
CareGuard Member

Everyone that I have dealt with at CareGuard has been friendly and extremely helpful.
CareGuard Member
Need more information?
Explore some of our most popular resources below.
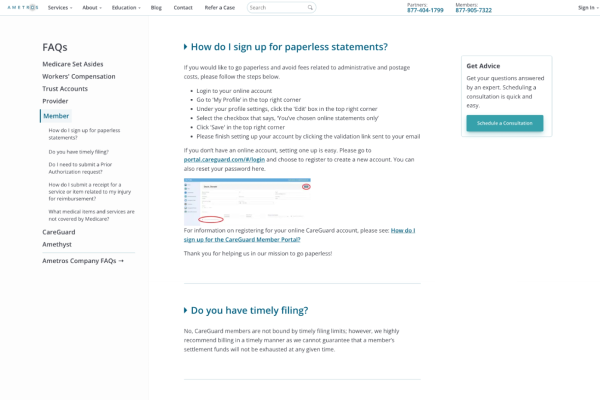
Member Frequently Asked Questions
Have a question about your CareGuard membership? Check out our Frequently
Asked Questions.

Provider Frequently Asked Questions
Read our collection of frequently asked questions for healthcare
providers.

Refer a Case
If you are looking to refer a case to us, please use our Refer a Case
form.

CareGuard Professional Administration
Learn more about Ametros' professional administration service, CareGuard.

CareGuard Portal
Login to the Ametros CareGuard member portal here.

Resource Center
Learn more about Workers' Compensation, Medicare Set-Asides and Ametros'
services, and more.


