Information for Healthcare Providers
About CareGuard
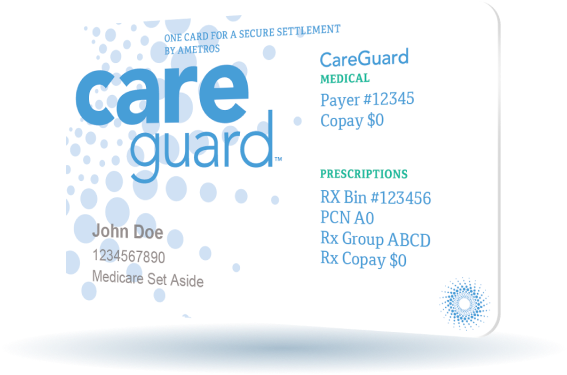
CareGuard is Ametros’ professional administration service your patient has selected to manage their medical fund account. Your patient sustained a work related or liability injury, which they subsequently settled. Upon settlement, they were granted funds to pay for their future medical care related to this injury. From this point on, CareGuard should be billed for all claims related to this injury. CareGuard is not an extension of Workers’ Compensation thus the same reporting rules, authorizations, and visit limits are not applicable. The services reimbursed from the MSA must be related to the members’ covered injury and, for a Medicare Set-Aside, be services that are covered by traditional Medicare.
Contact Us
Our Provider Services line, 1-877-905-7322 option 2, is available to check member eligibility and claim status from 9 a.m. to 6 p.m. EST Monday – Friday.
You may also email questions to: claims@careguard.com
Billing
Providers are obligated to bill against the MSA and “[p]roviders should also accept payment from professional administrators holding [MSA] funds. Providers should not bill Medicare where a third party holds and administers one of these MSA funds. For more information, please see:
Submitting Claims
CareGuard accepts claims typed on a CMS-1500 or UB-04. Please do not submit handwritten forms. Paper submissions should be computer generated or typed for scanning recognition. Handwritten claims may be rejected causing a delay in payment.
We highly recommend submitting claims via our electronic payer ID, 20572. This will provide a shorter turnaround time and increased accuracy.
Claims may also be mailed to the following address:
Please note, we are unable to accept faxed or emailed claims.
Please include the CareGuard Member ID in Box 1A of the CMS-1500 or Box 60 of the UB-04.
To receive reimbursement a provider must have an NPI that matches/is registered with an existing tax identification number. NPI requirements are federally mandated. Further information on NPI is available at CMS.gov
Claim Processing
Claims are typically processed within 10 business days and are paid using virtual credit cards (VCC).
The VCC will arrive in the mail and can be processed the same way you would process a patient’s credit card at the time of service. If your office does not accept credit cards, there is an option on the VCC to change your payment method to a check.
For problems processing the VCC, please call Data Dimensions at 631-648-6020 or email DDPaySupport@DataDimensions.com.
Claim Refunds
If a claim refund is required please follow the steps below:
Provider initiated refunds should include:
- Member ID, Name, and DOB
- DOS
- Reason for refund
- Copy of the EOR
Response to CareGuard initiated refund request should include:
- Copy of the letter you received
- Check made out to Ametros Financial Corporation FBO: (Member’s Name)
Mail to:
Prior Authorizations
Provider Authorization is NOT required for medical services but is recommended for services with a cost over $5,000. PT/OT/ST, radiology, and ESI do not require prior approval. There are no visit limits on therapies and no expiration dates for authorizations.
Requests for prior authorization may be faxed to 1-877-443-9344 or emailed to Claims@CareGuard.com.
We recommend using the CareGuard Prior Authorization form.
Download Ametros Prior Authorization Form
If you prefer using your own form, please include the following information:
- Member’s name, DOB, and CareGuard Member ID
- Rendering provider’s name
- Facility name
- Requested service with CPT codes
- Related diagnosis
- Estimated cost
DME items always require prior approval. Requests may be faxed to 877-443-9344 or emailed to DME@CareGuard.com.
Please include the following information on any requests:
- Member’s name, DOB, and CareGuard Member ID
- Member’s address and phone number
- Provider’s name, address, phone/fax/email
- HCPCS, quantity, description, and price
When submitting a claim, please include the case number provided by CareGuard in Box 23, prior authorization number, of the CMS-1500 form.

